Artificial Insemination
Watch our video about Artificial Insemination
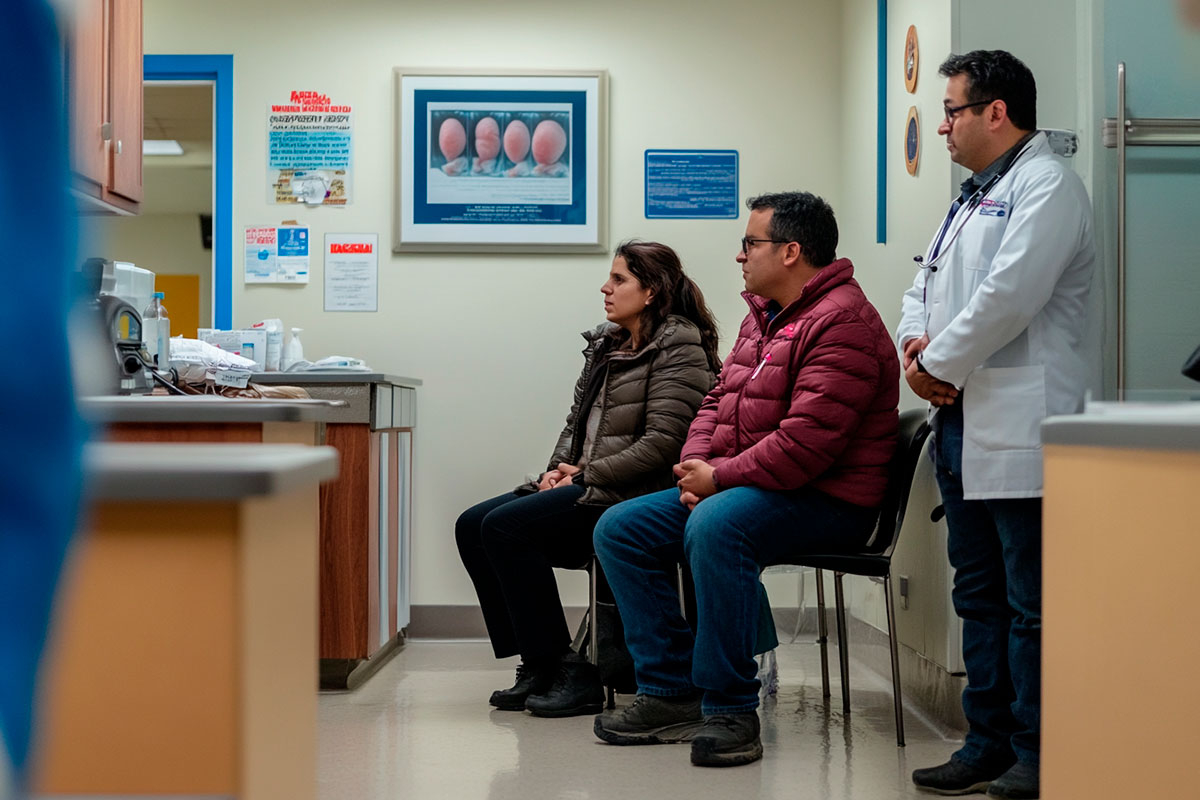
Intrauterine insemination (IUI) involves placing sperm directly into a woman’s uterus to enhance the chance of fertilization. Initially, the woman’s ovulation is tracked, either naturally or through medication. The sperm is processed in a lab to concentrate the healthiest cells, which are then inserted into the uterus via a catheter.
The procedure is quick, with minimal discomfort, and typically doesn’t require recovery time. Ovulation is closely monitored with ultrasounds to ensure the best timing for the insemination.
When Is IUI Recommended?
IUI is often recommended for individuals facing mild fertility challenges, such as low sperm count, ovulation disorders, or cervical mucus issues. It’s also a solution for single women and same-sex couples using donor sperm.
In cases of unexplained infertility, IUI can help, provided the woman’s fallopian tubes are clear. It’s generally a first-line fertility treatment, suitable when more invasive procedures aren’t immediately necessary.
Pre-IUI Care and Preparations
Before undergoing IUI, both partners typically undergo fertility testing to evaluate reproductive health. The woman’s cycle is closely monitored through hormone tests and ultrasounds to ensure ovulation occurs.
Lifestyle adjustments, including healthy eating, regular exercise, and avoiding harmful habits like smoking and alcohol, are encouraged. The medical team may also provide specific guidelines depending on individual health factors to optimize the chances of a successful insemination.
Conditions for the IUI Procedure
To qualify for IUI, the woman must ovulate regularly, either naturally or with the help of fertility medications. Clear fallopian tubes are essential for the sperm to reach the egg. Additionally, the sperm sample, whether from a partner or a donor, needs to meet quality standards, including a sufficient concentration of motile sperm.
IUI may not be appropriate for individuals with severe fertility issues, such as blocked fallopian tubes or significantly low sperm quality, where more advanced options like IVF are preferable.
The Role of Age in Intrauterine Insemination (IUI)
Age is a key determinant in the success rates of IUI. Women under 35 generally have higher success rates due to the quality of their eggs. After 35, fertility begins to decline, which impacts the overall success of the procedure.
Women over 40 may still attempt IUI, but doctors will evaluate ovarian reserves and provide tailored recommendations based on fertility levels. While age influences the outcome, additional fertility support or advanced treatments may be explored in later reproductive years.
Difference Between IUI and In Vitro Fertilization (IVF)
IUI and IVF are two distinct fertility treatments. In IUI, sperm is introduced directly into the uterus to allow fertilization to occur naturally. In IVF, eggs are retrieved from the ovaries, fertilized in a laboratory, and then transferred back to the uterus.
IVF is generally used for more complex fertility cases, including severe male factor infertility or blocked fallopian tubes, while IUI is less invasive and suitable for milder fertility challenges.
When Can I Take a Pregnancy Test After IUI?
After IUI, it’s important to wait 10 to 14 days before taking a pregnancy test. Testing too early might result in a false negative because it takes time for the embryo to implant and for pregnancy hormones to rise to detectable levels.
For a more accurate result, your doctor might recommend a Blood test to measure hCG levels, providing earlier confirmation of pregnancy.
What Are the Success Rates of IUI?
The success rates of IUI depend on factors such as the woman’s age, the quality of the sperm, and the underlying cause of infertility. For women under 35, the success rate ranges from 10% to 20% per cycle. After the age of 40, the success rates tend to decrease significantly.
It’s common to undergo multiple cycles of IUI, with doctors often recommending up to three or four attempts before considering more advanced fertility treatments like IVF.
Frequently Asked Questions
1. How many IUI cycles should I try before considering other treatments?
Doctors typically recommend trying 3 to 4 cycles before considering IVF or other treatments.
2. Is IUI painful?
No, the procedure is usually painless. Some women may experience mild discomfort similar to menstrual cramps.
3. Does IUI increase the chances of twins?
Yes, if ovulation is stimulated with medication, there is a higher chance of releasing multiple eggs, increasing the likelihood of twins.
4. Can I resume normal activities after IUI?
Yes, most women can return to their daily routines immediately after the procedure.
5. What should I do if the first IUI cycle doesn’t result in pregnancy?
If the first cycle isn’t successful, your doctor may adjust the treatment protocol and continue with additional cycles to increase the chances of success.